Diabetes is a persistent and long-lasting illness that takes place when the body cannot use the insulin it produces (diabetes type 2) or when the pancreas does not produce enough insulin (diabetes type 1), resulting in too much glucose in the bloodstream. [1]
According to the International Diabetes Federation,1 in 11 adults between 20 and 79 years have diabetes worldwide [2], being the major cause of important complications including kidney failure, blindness, heart attacks, and lower-limb amputations. [3]
Many therapies are currently available, including oral, injectable, or combined, depending on the type of diabetes, the disease’s evolution, and each personal case. Moreover, insulin, a hormone that moves glucose from the bloodstream into the body’s cells, is still recommended as the preferred treatment in many patients. [4]
Despite the various insulins available in the market, it is essential to consider that they need to be carefully prescribed, administered, and stored in a cool environment. Unfortunately, not all storage devices can easily and efficiently preserve insulin, negatively impacting its viability, potency, and biological activity.
What happens when insulin is not stored at a proper temperature?
Nowadays, very less is known about how people with diabetes store their insulin. Still, it is widely assumed that improper management can be due to a lack of understandable information and efficient store devices. Patients need to be aware that poor storage conditions will have a blood glucose-lowering effect with considerable health implications.
Here are some take-home messages that any diabetic patient need to know about insulin:
- Insulin formulations start to lose bioactivity (around 18% potency of decrease) after two weeks exposed to temperatures of +32°C and +37°C. [5]
- In the daily lives of many people with diabetes, insulin can be exposed to temperatures outside the recommended range to the extent that it can induce metabolic effects. This is essentially important for patients who take insulin several times a day when precise dosing is essential to achieve optimal outcomes. [6]
- Different insulin products can vary in peptide structure, formulation, and manufacturing methods, influencing their stability through different temperatures. [7]
- Many insulin brands provide unspecific or no further indications on how exposure to specific higher or lower temperatures for a particular time impacts insulin efficacy.
- There is little reliable information about the impact on insulin potency of shorter or repeated temperature deviations below or above the recommended storage conditions.
How can I store my insulin correctly?
The Food and Drug Administration’s (FDA) recommends that once insulin is taken out of the refrigerator and opened, it can be stored within +2°C/36°F and +25°C/77°F or +30C/86F, and used within 4 to 6 weeks. [8] According to the American Diabetes Association [9] and the National Diabetes Scheme [10], insulin should be stored under the following conditions:
- Do not store in extreme heat, extreme cold, or direct sunlight.
- The unopened insulin should not be frozen or stored in the freezer/chiller of the fridge.
- Keep the insulin you are using at room temperature (below 30 degrees Celsius). Once insulin has been opened, it can be discarded after 28 days (4 weeks).
- Use thermometers to monitor appropriate storage temperatures.
What options do I have to store my insulin?
To date, several products on the market offer broad protection for insulin pens and vials from heat when a fridge is not available. An insulated bag, case, wallet, or a cooling pouch are ideal for insulin transportation to avoid sudden temperature variations through sophisticated technologies like evaporation.
However, no further and reliable studies have been performed to see how stable insulin remains when it is stored within these bags or cases and if recommended temperatures can be maintained.
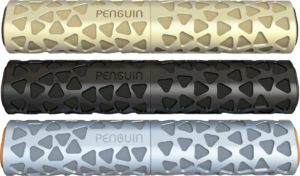
Fortunately, Penguin is a unique pen travel device that allows efficient, practical, and friendly insulin storage for any person with diabetes.
Bibliography
1.- Introduction: Standards of Medical Care in Diabetes—2021. (2020). Diabetes Care, 44(Supplement 1), S1–S2.
2.- IDF Diabetes Atlas 9th edition 2019. (2019). International Diabetes Federation.
3.- Diabetes. (2020, June 8). World Health Organization.
4.- Cahn, A., Miccoli, R., Dardano, A., & Del Prato, S. (2015). New forms of insulin and insulin therapies for the treatment of type 2 diabetes. The Lancet Diabetes & Endocrinology, 3(8), 638–652.
5.- Vimalavathini, R., & Gitanjali, B. (2009). Effect of temperature on the potency & pharmacological action of insulin. The Indian journal of medical research, 130(2), 166–169.
6.- Braune, K., Kraemer, L. A., Weinstein, J., et al. (2019b). Storage Conditions of Insulin in Domestic Refrigerators and When Carried by Patients: Often Outside Recommended Temperature Range. Diabetes Technology & Therapeutics, 21(5), 238–244.
7.- Heinemann, L., Braune, K., Carter, A., Zayani, A., & Krämer, L. A. (2020). Insulin Storage: A Critical Reappraisal. Journal of Diabetes Science and Technology, 15(1), 147–159.
8.- Center for Drug Evaluation and Research. (2017, September 19). Information Regarding Insulin Storage and Switching Between Products in an Emergency. U.S. Food and Drug Administration.
9.- Insulin Storage and Syringe Safety | ADA. (n.d.-b). American Diabetes Association. Retrieved April 9, 2021.
10.- Diabetes Australia. (2020, November 5). Insulin fact sheet – NDSS. National Diabetes Services Scheme.

